AI voice coach shows promise in psychotherapy for depression and anxiety
With scarce clinical resources unable to keep pace with elevated rates of mental illness, technological solutions could help decrease waitlists and disparities in access to therapy. Recent advances in artificial intelligence have fueled interest in the use of chatbots and virtual assistants for mental health treatment.

A new study led by researchers from University of Illinois Chicago, with collaborators at Washington University and Pennsylvania State University, finds that an AI voice assistant app delivering a form of psychotherapy can help patients with mild depression and anxiety. The article, published in Translational Psychiatry, reports changes in brain activity along with improved depression and anxiety symptoms after using the AI voice assistant, called Lumen, for eight sessions of problem-solving therapy.
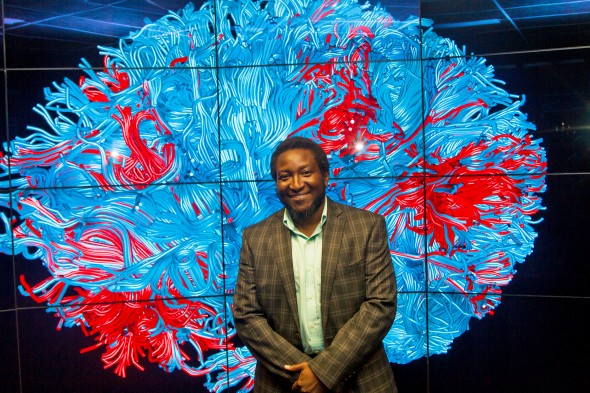
The results of this pilot study, the first to test an AI voice-based virtual coach for behavioral therapy, offer encouraging evidence that virtual therapy can play a role in filling the gaps in mental health care, said co-first author Dr. Olusola A. Ajilore.
“We’ve had an incredible explosion of need, especially in the wake of COVID, with soaring rates of anxiety and depression and not enough practitioners,” said Ajilore, professor of psychiatry at UIC. “This kind of technology may serve as a bridge. It’s not meant to be a replacement for traditional therapy, but it may be an important stop-gap before somebody can seek treatment.”
Ajilore and study senior author Dr. Jun Ma, the Beth and George Vitoux Professor of Medicine at UIC, received a $2 million grant in 2020 to develop an AI coach called Lumen for treatment of mild-to-moderate anxiety and depression. Lumen, which operates as a skill in the Amazon Alexa application, delivers evidence-based problem-solving therapy, which helps patients to develop positive mindset and skills for solving daily problems that cause emotional distress.
“It’s about changing the way people think about problems and how to address them, and not being emotionally overwhelmed,” Ma said. “It’s a pragmatic and patient-driven behavior therapy that’s well established, which makes it a good fit for delivery using voice-based technology.”
After developing Lumen with their colleagues at Washington University in St. Louis and Pennsylvania State University, the researchers recruited 63 patients for a pilot study of its effect on depression and anxiety symptoms and activity in brain areas previously shown to be associated with the benefits of problem-solving therapy. Two-thirds of the patients used Lumen on a study-provided iPad for eight problem-solving therapy sessions, with the rest serving as a “waitlist” control receiving no intervention.
After the intervention, the Lumen group showed decreased scores for depression, anxiety and psychological distress compared with the control group. The Lumen group also showed improvements in problem-solving skills that correlated with increased activity in the dorsolateral prefrontal cortex, a brain area associated with cognitive control.
In combination, the results provide a promising link between neurological and behavioral effects that supports further investigation of the intervention.
“With this experimental therapeutics approach, you have an idea of why things work,” Ajilore said. “More importantly, you have an idea for whom these things work best for. In precision psychiatry, the mantra is finding the right treatment for the right person at the right time. These neural targets might actually serve as a biomarker for who will do best with this type of treatment.”
The intervention also showed especially promising results for women and underrepresented populations. Seeing effects in these populations was gratifying for the researchers, who designed and tested Lumen with feedback from these groups.
“If this form of treatment might actually offer, not only just access, but greater benefits to ethnic and racial minorities, that’s very meaningful,” Ma said.
“Another lesson of this pilot is that if you’re trying to design a digital mental health intervention to help a diverse patient population, you have to have that diverse patient population involved in the development of that intervention in order for them to get the maximum benefit from it,” Ajilore said.
Building on the success of the pilot study, the research group is now conducting a larger trial comparing use of Lumen with both a control group on a waitlist, and patients receiving human-coached problem-solving therapy. But they stress that the virtual coach doesn’t need to perform better than a human therapist to fill a desperate need in the mental health system.
“The way we should think about digital mental health service is not for these apps to replace humans, but rather to recognize what a gap we have between supply and demand, and then find novel, effective and safe ways to deliver treatments to individuals who otherwise do not have access, to fill that gap,” Ma said. “Then there is more of an opportunity to think about how we allocate our very limited resources so that we can serve more patients who need care.”
The team will also consider integrating the dramatic progress recently made in AI language models, such as ChatGPT, for future iterations of Lumen or other digital interventions. But with all such AI uses in medicine and psychiatry, the hype must be confirmed with careful research.
“In the wake of this AI revolution and large language models over the last year, having a solid evidence base and careful, rigorous scientific work behind this approach is absolutely what’s needed before we actually start deploying it with our patients,” Ajilore said.
Categories
Featured Academic Research, Health Sciences Colleges, Research, UIC today
Topics
artificial intelligence, mental health, psychiatry, technology