‘Junk DNA’ offers clue to stopping cancer drug’s vascular damage
An unfortunate side effect of some cancer treatments is cardiovascular dysfunction, leading patients to trade one dangerous disease for another. Sunitinib, a tyrosine kinase inhibitor used to treat kidney, gastrointestinal and pancreatic cancers, can cause vascular dysfunction and cardiac abnormalities, but scientists are unsure why.
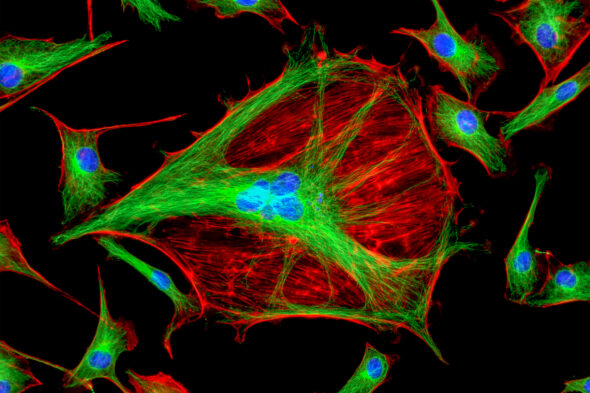
In new research, a collaborative team led by UIC’s Sang-Ging Ong uncovered the mechanism for this toxicity by testing how sunitinib affects the protective layer inside blood vessels. The group looked at how the drug affects endothelial cells, which line the interior of arteries and veins, zeroing in on a particular type of cellular signal called long non-coding RNA.
These RNAs are produced by what was once called “junk DNA,” segments of DNA that don’t carry instructions for producing proteins. However, recent studies have found that these stretches can play an important biological role, encoding RNA molecules that regulate important cellular processes.
Ong’s team found that sunitinib depleted a particular long non-coding RNA called HAS2-AS1 in endothelial cells. Further experiments showed that this RNA is important for maintaining the glycocalyx, the outermost structure that protects endothelial cells from damage, through its role in regulating the production of hyaluronic acid.
In mice treated with sunitinib, the researchers saw a similar pattern of damage to the glycocalyx of endothelial cells. But giving the mice hyaluronic acid in combination with the drug prevented the vascular damage caused by the therapy. The results suggest that hyaluronic acid, a substance found in anti-wrinkle cosmetic products, could be a promising tactic to prevent the side effects of this cancer treatment.
“The story is pretty interesting because, first, we demonstrated that these long non-coding RNAs are involved in cancer-induced toxicity,” said Ong, an assistant professor of pharmacology and regenerative medicine at UIC. “And secondly, we showed that the extracellular matrix is an important determinant of this dysfunction. Usually, people think that the extracellular matrix is solely a static structural support of cells, but in this case, we showed that it plays a role in terms of protecting the vasculature.”
The study is published in Cardiovascular Research, and also included UIC co-authors Sarath Babu Nukala, Jordan Jousma, Gege Yan, Zhenbo Han, Youjeong Kwon, Yoonje Cho, Sandra Pinho and Dr. Jalees Rehman. The work was funded by NIH grants R00HL130416, R01HL148756, and R01HL162584 in addition to external collaborative funding.