US dentists out prescribe UK dentists when it comes to opioids
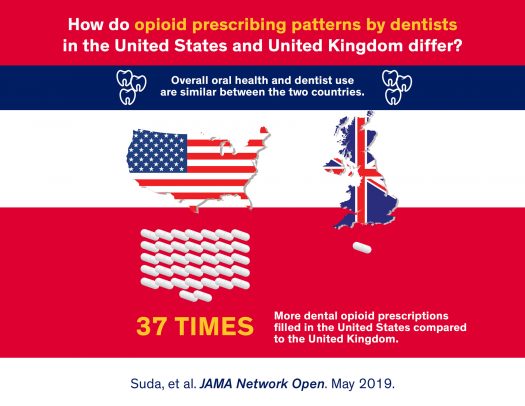
Researchers from the University of Illinois at Chicago have found that dentists practicing in the U.S. write 37 times more opioid prescriptions than dentists practicing in England. And, the type of opioids they prescribe has a higher potential for abuse.
Their findings, which are reported in JAMA Network Open, suggest that measures to reduce opioid prescribing by dentists, who are among the top prescribers of opioids in the U.S., should be discussed by policymakers and professional associations.
The study was, in part, a collaboration between UIC’s Colleges of Pharmacy and Dentistry, and the University of Sheffield.
UIC’s Katie Suda, the corresponding author of the study, says that the degree to which prescribing patterns differ between dentists in the two countries, which have similar oral health and dental utilization, is eye-opening.
“To see such a difference between two groups of dentists in countries with similar oral health and use of dentists is an indicator that opioid prescribing practices in the U.S. warrant a second look,” said Suda, associate professor of pharmacy systems, outcomes and policy at the UIC College of Pharmacy. “This study tells us that efforts to adopt national guidelines for treating dental pain and for promoting conservative opioid prescribing practices among dentists in the U.S. should be a priority and should be included as part of more comprehensive judicious opioid prescribing strategies.”
To study dental provider opioid prescribing practices in the two countries, Suda and her colleagues analyzed nationally-representative databases from both countries of prescriptions dispensed from retail pharmacies, including community and mail service pharmacies, and outpatient clinic pharmacies in 2016, which is considered to be a peak point in the U.S. opioid crisis.

They found U.S. dentists wrote 37 times more opioid prescriptions in 2016 — 1.4 million in the U.S. compared to only 28,000 in England. This finding remained even when the researchers adjusted for differences in population size and number of dentists.
They also found that U.S. dentists prescribed a much wider range of opioids, where dentists in England only prescribed one — a codeine derivative called dihydrocodeine, which is the only opioid included in the formulary used by their National Health Service. In the U.S., the most commonly prescribed opioids were hydrocodone-based, followed by codeine, oxycodone and tramadol. One in ten opioids prescribed by U.S. dentists were opioids with a high potential for abuse and diversion, such as oxycodone and long-acting opioids. Dentists in England did not prescribe these opioids.
“Dentists need to be part of the opioid conversation,” said co-author Dr. Susan Rowan, executive associate dean and associate dean for clinical affairs at the UIC College of Dentistry. “It is common for people to overlook dental issues until pain becomes severe and major interventions are needed. Pain killers are often an essential part of dental care and provider flexibility in choice is important, but this study shows us there is room for dental care providers to contribute to and inform abuse reduction programs.
“This data should be a wakeup call to individual dental practices and collaborative organizations of dental care providers to push the envelope towards greater efforts to reduce opioid prescribing or patients’ potential for abuse,” Rowan said.
“I was shocked to discover the high level of opioid prescribing of my U.S. dental colleagues. Particularly, when there is good evidence that NSAIDs and acetaminophen are as good or better than opioids for treating dental pain and don’t cause the unpleasant side-effects, addiction and misuse problems associated with opioids,” said co-author Dr. Martin Thornhill, professor of translational research in dentistry at the University of Sheffield. “UK dentists manage exactly the same pain problems as their U.S. colleagues and achieve high levels of patient satisfaction using NSAIDs and acetaminophen, without the need to resort to opioids.”
This research was supported by the Agency for Healthcare Research and Quality (R01HS25177) and the National Institutes of Health’s National Center for Advancing Translational Sciences (UL1TR002003).
Additional co-authors include Gregory Calip and Hajwa Kim of UIC, Dr. Michael Durkin of Washington University, Dr. Walid Gellad of the University of Pittsburgh, and Dr. Peter Lockhart of Carolinas Medical Center.