Transforming clinicals to meet COVID reality
When word came down from the University of Illinois System in mid-March that all in-person classes would migrate online to prevent the spread of coronavirus, it presented a special challenge for nursing clinical instructors.
How do you give nursing students a clinical experience without being in a clinic?
Susan Kilroy knew part of the solution could be virtual simulations of clinical experiences. As director of the UIC Nursing Clinical Learning Resource Center, Kilroy, oversees the M. Christine Schwartz Experiential & Simulation Laboratory in Chicago as well as simulation labs in Springfield and Urbana.
“With the way everything unfolded, we had to quickly transition from in-person clinical to virtual simulation experiences,” Kilroy said.
The university system added a second week to spring break, affording faculty an extra week to transition their classes to a virtual format. Kilroy worked with lab coordinators Lynn Ortiz in Chicago, Peggi White in Urbana, and Christine Freer in Springfield to scour the Internet for videos and other resources on virtual simulation, then uploaded them to an online library for faculty and staff.
“Our goal is to replicate the experiences our students would typically receive in clinical settings or the lab with virtual software, and for our graduating seniors, to give them the skills they need to graduate and enter the workforce,” says Catherine Vincent, associate dean for academic affairs.
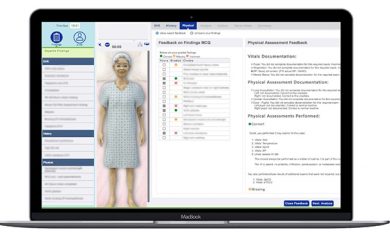
Using a virtual simulation computer package called iHuman, more than 400 bachelor’s degree students and 280 graduate-level students will be able to practice skills on an avatar patient. The students can read the patient’s chart, ask questions, and even check the patient’s heartbeat by putting their cursor over the patient’s heart. Via videoconference, faculty can ‘meet’ with students before seeing the patient and a debrief after, just as they would in a typical clinical situation.
Creative clinicals
Telehealth is another way some DNP students will be able to get clinical hours. Mental health nurse practitioner students, for instance, will be able to use videoconferencing software to call standardized patient in their homes.
Janey Kottler, formerly Jubas, who is an instructor for the community health course, says some of her students are gaining clinical hours by creating public education materials for different populations. For instance, one group is creating fliers on hand hygiene. Another is doing a pre-recorded video and Powerpoint presentation for an elderly LGBTQ group.
“Because this is a public health emergency, this is a perfect opportunity to do public health teaching from a safe distance,” Kottler says.
As useful as virtual experiences are, certain clinical hours cannot be replaced with simulation. For instance, neonatal nurse practitioner students have to spend at least 500 hours of direct care working with a neonatal nurse practitioner or physician in a Neonatal Intensive Care Unit.
Kilroy says special skills days may also be offered later for students who want extra practice or need to demonstrate competency in front of their instructors.
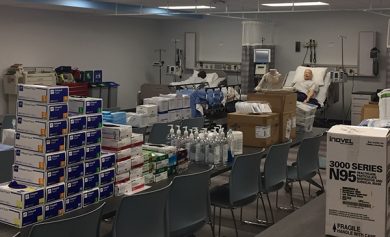
In the meantime—when students are not on campus—physical materials in the simulation labs are being put to good use. Gowns, gloves, masks, eye protectors, thermometer covers and hand sanitizer were donated to hospital workers. Three mid-fidelity manikins from the M. Christine Schwartz Experiential & Simulation Laboratory are also on loan to UI Hospital to cross-train outpatient clinic nurses to care for patients in the inpatient setting.
