Emotion-processing networks disrupted in sufferers of depression
Regions of the brain that normally work together to process emotion become decoupled in people who experience multiple episodes of depression, neuroscientists report. The findings may help identify which patients will benefit from longterm antidepressant treatment to prevent the recurrence of depressive episodes.
The study, led by researchers at the University of Illinois at Chicago, is published in the journal Psychological Medicine.
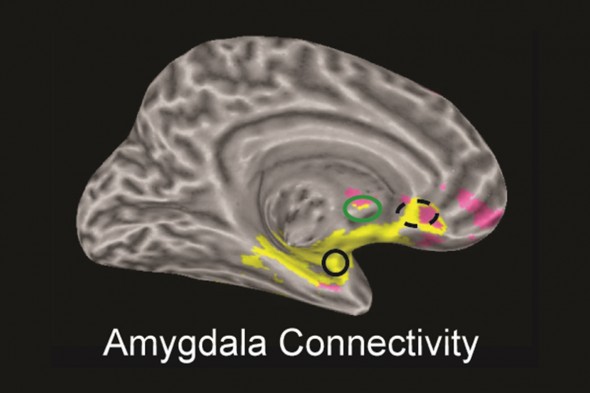
Regions of the emotional network that connect with the amygdala (black circle) in people without depression are highlighted in yellow. The areas of pink highlight regions that have reduced connectivity with the amygdala in people who experience multiple episodes of depression.
“Half of people who have a first depressive episode will go on to have another within two years,” says Scott Langenecker, associate professor of psychiatry and psychology at UIC and corresponding author on the study.
Disruptions in the network of areas of the brain that are simultaneously active during problem-solving and emotional processing have been implicated in several mental illnesses, including depression. But in addition, “hyperconnectivity,” or too much connection, within the “resting network,” or areas active during rest and self-reflection, has also been linked to depression.
“If we can identify different network connectivity patterns that are associated with depression, then we may be able to determine which are risk factors for poorer outcomes down the line, such as having multiple episodes, and we can keep those patients on preventive or maintenance medication,” Langenecker explained. “We can also start to see what medications work best for people with different connectivity patterns, to develop more personalized treatment plans.”
In previous research, Langenecker found that the emotional and cognitive brain networks were hyperconnected in young adults who had depression. Areas of the brain related to rumination – thinking about the same thing over and over again – a known risk factor for depression, were also overly connected in adolescents who had experienced depression.
In the new study, Langenecker said he and his coworkers wanted to see if different patterns of network-disruption would show up in young adults who had experienced only one episode of depression versus several episodes.
The researchers used functional magnetic resonance imaging, or fMRI, to scan the brains of 77 young adults (average age: 21.) Seventeen of the participants were experiencing major depression at the time of the scan, while 34 were currently well. Of these 51 patients, 36 had experienced at least one episode of depression in the past, and these individuals were compared to 26 participants who had never experienced a major depressive episode. None were taking psychiatric medication at the time they were scanned.
All fMRI scans were done in a resting state — to show which areas of the brain are most synchronously active as one relaxes and lets their mind wander.
The researchers found that the amygdala, a region involved in detecting emotion, is decoupled from the emotional network in people who have had multiple episodes of depression. This may cause emotional-information processing to be less accurate, Langenecker said, and could explain “negative processing-bias” in which depression sufferers perceive even neutral information as negative.
The researchers also saw that participants who had had at least one prior depressive episode — whether or not they were depressed at the time of the scan — exhibited increased connectivity between the resting and cognitive networks.
“This may be an adaptation the brain makes to help regulate emotional biases or rumination,” Langenecker said.
“Since this study provides just a snapshot of the brain at one point in time, longer-term studies are needed, to determine whether the patterns we saw may be predictive of a future of multiple episodes for some patients and might help us identify who should have maintenance treatments and targets for new preventive treatments,” he said.
Rachel Jacobs, Alyssa Barba, Jennifer Gowins, Heide Klumpp, Lisanne Jenkins, Dr. Olusola Ajilore and Dr. K. Luan Phan of the UIC College of Medicine, and Dr. Brian Mickey, Dr. Marta Pecina, Margaret Sikora, Kelly Ryan, David Hsu, Robert Welsh and Jon-Kar Zubieta of the University of Michigan are co-authors on the paper.
This study was funded in part by the UIC Center for Clinical and Translational Science and grants RO1 Q2 601, MH091811 and RO1 MH101487 from the National Institutes of Health.
