Rural medicine program helps bridge health care gap

Rural medicine student Mina Tanaka teaches third- and fouth-graders from the Karuk tribe how origami relates to being a good health care provider.
Mina Tanaka’s training experience is different from other fourth-year students in her medical program.
While her classmates in Rural Medical Education at the College of Medicine’s Rockford campus spend four months at hospitals and clinics in small communities across Illinois, Tanaka is the first to train on a Native American reservation.
As the RMED program expands next fall from 15 to 25 students, there will be more opportunities for students to train in Native American communities. Students will also have the chance to explore specialties such as surgery or psychiatry.
A high school mission trip to a Native American reservation in South Dakota was enough to convince Tanaka that she wanted to dedicate her career to underserved populations.
“It sparked my interest, seeing the disparity on the reservation compared to my suburban life,” said Tanaka, who lived in Skokie. “Rural medicine and native health are two areas that are very underserved.”
She left the Rockford campus Sept. 1 to start her four-month preceptorship working with the Karuk tribe in Northern California. She’s training at the Orleans Medical Clinic, which had no doctor for four months last year until its sole physician was hired in February.
“It’s an interesting dynamic,” she said. “We serve a lot of tribal members, and some hippies seeking alternative lifestyles away from the city. But they’re all underserved, lower-income patients.”
Tanaka is immersing herself in the community, visiting schools to promote health care careers. “I want to talk to as many students as possible and help empower them to think about health professions,” she said.
She doesn’t have cell phone reception and must drive two hours to shop. But living among the tribe has been an invaluable experience, she said.
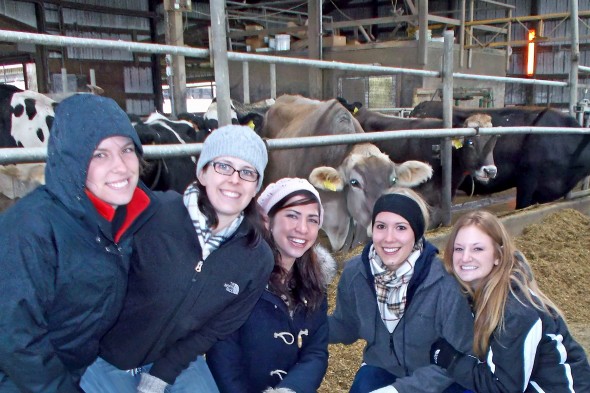
Medical students Mary Ayers (from left), Kendall Marszalek, Jennah LaHood, Laura
Hulteen and Kelley Williams.
“I’m getting used to the remoteness. It’s really gorgeous here. I’ve learned a lot about the tribe and its customs. It’s been really eye opening for me in a lot of ways.”
Commitment to serve rural areas
More than 200 students have graduated from the RMED program over the past 20 years, with 75 percent practicing primary care in rural areas, said Michael Glasser, program director. The Rockford campus also offers a College of Pharmacy program with a rural focus.
“There’s a shortage of physicians, particularly in rural areas,” he said. Most RMED students are recruited from rural Illinois, Glasser said, because they’ll be more likely to return to serve their community.
But a rural background doesn’t guarantee acceptance into the program — students must impress the RMED recruitment and retention committee, which includes health department directors, hospital CEOs, dairy farmers and rural physicians.
“The committee makes the decision of who gets admitted,” said Glasser, associate dean of the National Center for Rural Health Professions. “They are from rural communities and know who will be best to serve rural Illinois.”
In addition to the medical curriculum, students attend monthly seminars on rural medicine, alternative medicine, community health and other topics.
They complete a four-month preceptorship at one of 25 partner sites in Illinois communities, from Galena to Metropolis and Macomb to Watseka — a list that could expand to include Native American communities.
Helping out at home
Kendall Marszalek is completing a four-month preceptorship at the Midwest Medical Center in her hometown of Galena. The critical access hospital has 25 beds, an ER and a clinic.
The medical center has limitations — staff members cannot perform major surgeries or large orthopedic procedures such as hip replacement. Patients must travel more than an hour for major procedures, she said.
“Not everybody has access to drive and they have to rely on family members,” she said.
Marszalek knew she wanted to work in a rural community after shadowing a Galena family doctor during her undergraduate studies.
“The experience was more or less ‘picturesque old country doctor,’” she said. “We did home visits, visited nursing homes and had a lot of exposure in the community. I knew I wanted to do family medicine because of the people.”
Marszalek plans to practice in a rural community in northwest Illinois. “I’m not sure if I want to come back home, but a community with less than 10,000 people would be ideal,” she said.
Third-year rural medicine student John Mihelcic wants to practice back home in Staunton, a community of 5,000 residents between Springfield and St. Louis.
“The program gave me even more drive to return to a rural practice than when I first started it,” said Mihelcic, who received his bachelor’s in molecular and cellular biology at the Urbana-Champaign campus. “I saw the impact that some of the primary doctors have in the community and that I would be able to contribute positively in these rural areas.”
RMED students work closely with rural pharmacy students, which helps build interprofessional ties early in their careers. “Being able to see what they’re working on has been really eye-opening,” Mihelcic said.
The RMED program provides more culturally diverse training for physicians, Marszalek said.
“It definitely opens our eyes to more issues than you might see if working in just one specialty. “It gives you an edge to understand the issues in culturally diverse communities and ways to solve them.”

